Rationale: Drug-inducing adverse effects may be critical and fatal. There is a reported serious cardiovascular (CV) presentation with sildenafil. Mitral stenosis (MS) is the most common cause of valvular atrial fibrillation (AF) and flutter. Brugada syndrome (BrS) is a genetic disorder with abnormal electrical activity within the heart that carries a higher risk for ventricular fibrillation and sudden death. Hiatal hernia is a herniation of intra-abdominal contents into the thorax. There is a durable relationship between COVID-19 infection and ischemic heart disease.
Patient concerns: A 53-year-old, married Egyptian male teacher, mechanically replaced mitral valve (MV) patient was presented to the physician outpatient clinic with intermittent angina within two weeks’ of post-oral sildenafil tablets and COVID-19 pneumonia.
Diagnosis: High lateral ischemia and passed sildenafil-inducing inferior infarction with variable atrial fibro-flutter block, alternative right bundle branch block (RBBB) beat with type II BrS in mechanically replaced MV with recent hiatus hernia and COVID pneumonia.
Interventions: Cardiothoracic surgery, chest X-ray, electrocardiography, echocardiography, and oxygenation.
Outcomes: There is a good outcome despite numerous noteworthy serious risk factors.
Lessons: High lateral ischemia, passed inferior myocardial infarction (MI), variable atrial fibro-flutter block, RBBB beat, BrS, hypocalcemia, recent hiatus hernia, and COVID pneumonia in the mechanically replaced MV are a serious constellation of risk factors. Alternative RBBB beat with type II BrS is newly described. BrS may be transient. Hypocalcemia and Wavy triple ECG sign (Yasser’s sign) are confusing issues for ischemic heart disease.
sildenafil, ischemic heart disease, bundle branch block, Brugada syndrome, mitral valve disease, atrial fibro-flutter, COVID-19 pneumonia
CV: cardiovascular; MS: mitral stenosis; BrS: Brugada syndrome; RBBB: right bundle branch block; CAS: coronary artery spasm; MI: myocardial infarction; MV: mitral valve; AF: atrial fibrillation; BBB: bundle branch block; CRS: cytokine release syndrome; VR: ventricular rate; BP: blood pressure; MVR: mitral valve replacement; MVA: mitral valve area; CBC: complete blood count; CRP: C-reactive protein; RBS: random blood sugar
Drug-inducing adverse effects may be critical and fatal [1]. Angina, coronary artery spasm (CAS), and myocardial infarction (MI) are reported serious cardiovascular (CV) presentations with sildenafil [2]. Mitral valve (MV) stenosis is the most frequent cause of valvular atrial fibrillation (AF). Mitral stenosis (MS) is the most common cause of valvular AF [3]. The left atrial enlargement due to constant pressure and volume overload, the prevalence of AF is the pathogenesis mechanism of MS [4]. Atrial flutter is usually a transitional rhythm to either sinus rhythm or AF. The management of atrial flutter is overall very similar to that of AF [5]. The association between AF and bundle branch block (BBB) was reported. The prevalence of AF is higher in patients with BBB than without BBB but with no significant increase in mortality or length of stay [6]. Brugada syndrome (BrS) is a genetic disorder with abnormal electrical activity within the heart. The syndrome has a serious risk for ventricular fibrillation and sudden death in a normal heart. Three classes were identified; coved type (class I) has a coved type of ST-segment elevation with ≥2 mm (0.2 mV) J-point elevation and a gradually descending ST-segment followed by a negative T-wave [7]. Hiatal hernia is a herniation of intra-abdominal contents into the thorax. They can be classified into type I-IV based on different herniation grades. The symptoms can range from chest pain in the mild types to respiratory, hemodynamic compromise, and strangulation in the advanced types [8]. Thrombosis is one of the most common CV complications among COVID-19 patients [9]. Multiple mechanisms have been suggested for cardiac damage in the COVID-19 epidemic. The systemic inflammatory response in severe COVID-19 is the producing high levels of cytokines causing cytokine release syndrome (CRS) that can injure multiple tissues, involving vascular endothelium and cardiac myocytes [10].
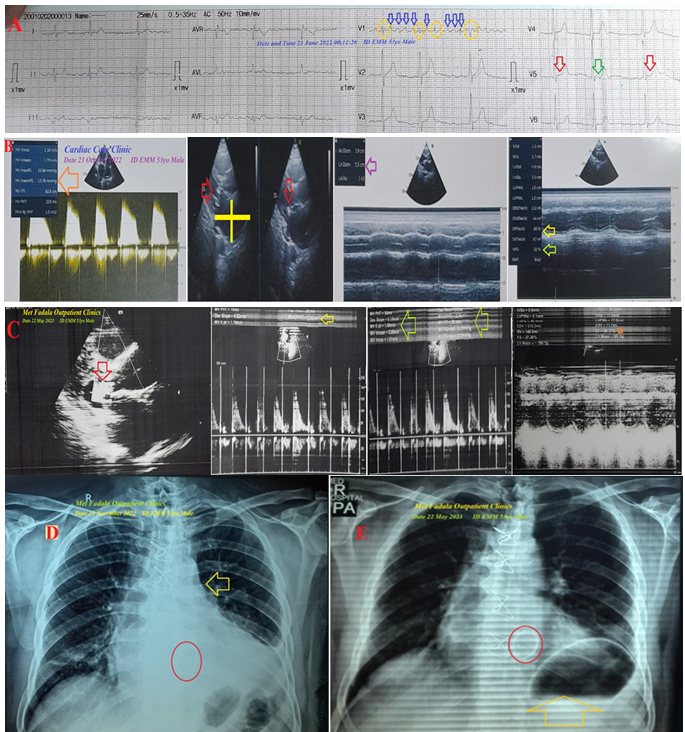
A 53-year-old, married Egyptian male teacher patient was presented to the physician outpatient clinic with angina. The angina is intermittent and relevant to frequent doses of sildenafil in the last two weeks. There is a history of recent psycho-familial troubles. The patient also gave a history of recent COVID-19 pneumonia within the past 17 days. He had a history of tight severe MS due to rheumatic fever. He underwent open heart surgery 1 year ago with a mechanically replaced MV. The patient continued on warfarin tablets (5 mg, OD, with follow-up with serial INR). Tachypnea, numbness, and paresthesia of extremities were associated symptoms. The patient denied a history of other relevant diseases, drugs, or other special habits. Informed consent was taken. Upon general physical examination, the patient appeared irritable and distressed with an irregular pulse rate of VR 70 bpm, blood pressure (BP) of 110/70 mmHg, respiratory rate of 21 bpm, a temperature of 36.5°C, and pulse oximeter of oxygen (O2) saturation of 97%. Tests for latent tetany were positive. The clicking sound of the mechanical MV was heard without auscultation on chest auscultations. Currently, the patient has refused to be referred to the ICU for angina and variable atrial fibro-flutter block in mechanical mitral valve replacement (MVR). Initially, the patient was treated with O2 inhalation by O2 generator (100% by nasal cannula, 5 L/min). The patient was managed at home with SC enoxaparin 80 mg, BID), aspirin tablet (75 mg, initially 4 tablets then OD), clopidogrel tablets (75 mg, initially 4 tablets then OD), atorvastatin tablets (20 mg, nightly, OD), and warfarin tablet (5 mg, OD) were added. The patient was daily monitored for temperature, pulse, blood pressure, ECG, and O2 saturation. The initial ECG tracing was done within a few months before the open-heart surgery intervention and mechanical MVR showed variable atrial fibro-flutter block (VR of 78) with Wavy double ECG sign or Yasser’s sign (V5) (Figure 1A). The perioperative echocardiography showed thickened MV leaflets especially, tips, diastolic dooming, restricted mobility, tight MS with MV area (MVA) 1cm2, peak/mean gradient 22/13, mild mitral regurgitation, thickened subvalvular apparatus, Wilkins score 13/16, mitral annulus 4.3 cm, thicken aortic valve with mild aortic regurgitation, markedly dilated left atrium, moderate tricuspid regurgitation, and good systolic function (Figure 1B). The echocardiography was repeated within 6 months post-mechanical MVR showing functioning MV prosthesis, moderate aortic regurgitation, still dilated left atrium, and good systolic function with EF of 68% (Figure 1C). The CXR film was done within two weeks before the open-heart surgery intervention and mechanical valve replacement showing a round shadow of mechanical prosthetic MV, still cardiomegaly, and slight mitralization of the heart (Figure 1D). The CXR film was repeated within 6 months post-mechanical MVR showing a round shadow of mechanical prosthetic MV and left retrocardiac opacity with gas-fluid level (Figure 1E).
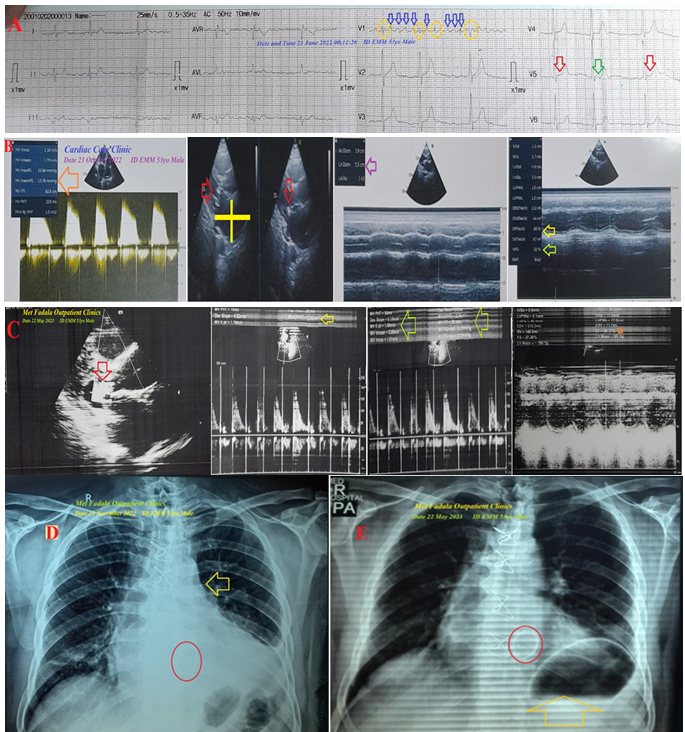
Figure 1: A) ECG tracing was done within a few months before the open-heart surgery intervention and mechanical MVR showed variable atrial fibro-flutter block (VR of 78; dark blue arrows and golden circles) with Wavy double ECG sign or Yasser’s sign (V5; green and red arrows). B) Perioperative echocardiography showed thickened MV leaflets (red arrow), tight MS with MVA (pink arrow), markedly dilated left atrium (yellow cross), and good systolic function with EF of 62% (golden arrow) and FS of 32% (lime arrow). C) Echocardiography was done within 6 months post-mechanical MVR showing functioning MV prosthesis (red arrow), with MVA (golden and lime arrows), dilated left atrium, and good systolic function with EF of 68% (orange arrow) and FS of 32% (lime arrow). D) CXR film was done within two weeks before the open-heart surgery intervention and mechanical MVR showed a round shadow of mechanical prosthetic MV (round red circle), still cardiomegaly, and slight mitralization of the heart (golden arrow). E) CXR film was done within 6 months post-mechanical MVR showing a round shadow of mechanical prosthetic MV (round red circle) and left retrocardiac opacity with gas-fluid level (golden arrow).
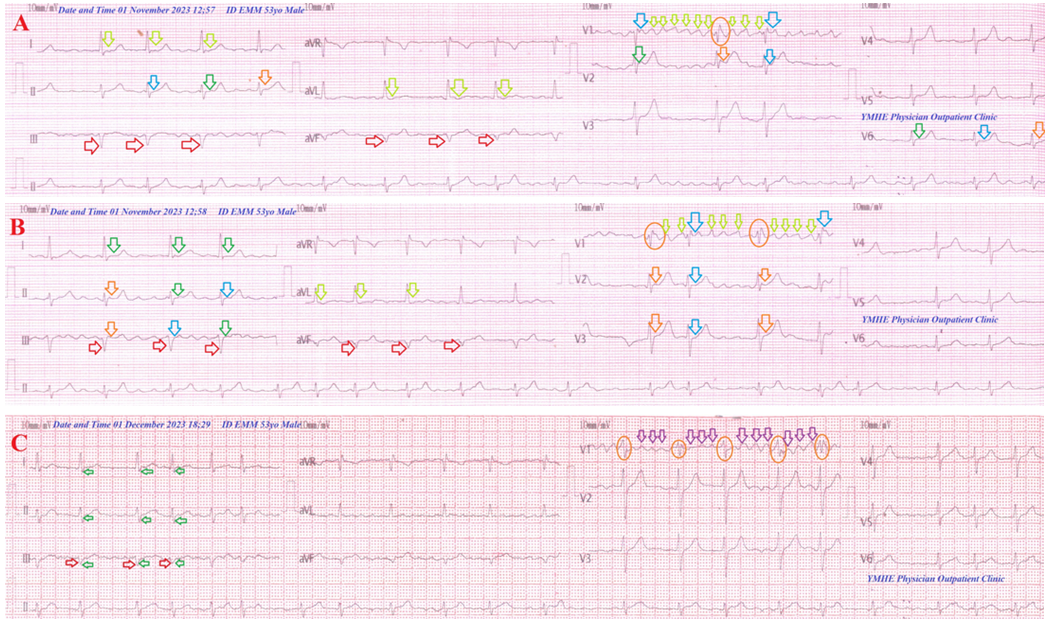
The second ECG tracing was taken on the current presentation showing variable atrial fibro-flutter block (VR of 72), high lateral ST-segment depression (I and aVL), inferior pathological Q waves (III and aVF), alternative right bundle branch block (RBBB) beat with type II BrS (V1) with Wavy triple ECG sign or Yasser’s sign (II, V2, and V6) (Figure 2A). The third ECG tracing was taken within 1 min of the above ECG tracing showing variable atrial fibro-flutter block (VR of 78), ST-segment depression in aVL lead with normalization of ST-segment depression in I lead, inferior pathological Q waves (III and aVF), alternative RBBB beat with type II BrS (V1), and Wavy triple ECG sign or Yasser’s sign (II, III, V2, and V3) (Figure 2B). The fourth ECG tracing was taken within 30 days of the last 2 tracings and treatment showed controlled fixed atrial fibro-flutter block (VR of 90), SISIISIII pattern, inferior pathological Q waves (III and aVF), and RBBB with no type II BrS (V1) (Figure 2C). The initial complete blood count (CBC): Hb was 12.1 g/dL, RBCs 4.7 × 103/mm3, WBCs 9.2 × 103/mm3 (neutrophils 62%, lymphocytes 34%, monocytes 4%, eosinophils 0%, and basophils 0%), and platelets 157 × 103/mm3. CRP was high (7 g/dL). SGPT (24 U/L) and SGOT were normal (19 U/L). Serum albumin was normal (3.6 g/dL). Serum creatinine (0.6 mg/dL) and blood urea (13 mg/dl) were normal. RBS was normal (122 mg/dL). Plasma sodium was high (143 mmol/L). Serum potassium was normal (4.5 mmol/L). Ionized calcium was slightly low (0.9 mmol/L). The troponin test was negative. High lateral ischemia and passed sildenafil-inducing inferior infarction with variable atrial fibro-flutter block, alternative RBBB beat with type II BrS in mechanically replaced MV with recent hiatus hernia and COVID pneumonia was the most probable diagnosis. Within 5 days of the above management, the patient finally showed nearly dramatic clinical and mostly electrocardiographic improvement. The patient was maintained after clinical stabilizations and continued on aspirin tablets (75 mg, OD), clopidogrel tablets (75 mg, OD), warfarin tablets (5 mg, OD), and atorvastatin tablets (20 mg, OD). Oral calcium and vitamin D preparation were prescribed for two weeks. Further recommended cardiac follow-up was advised.
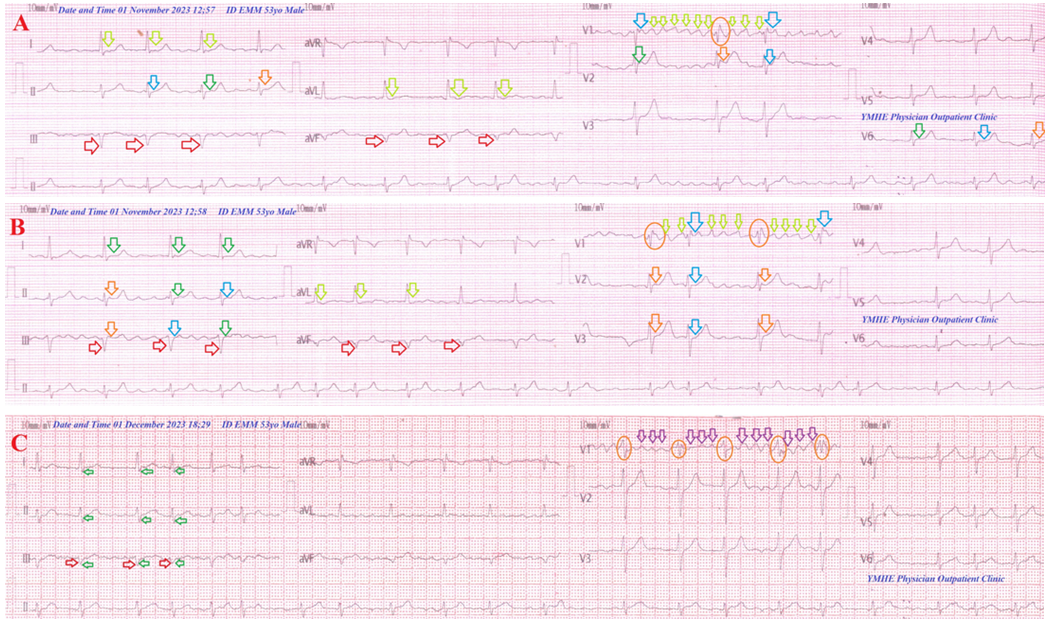
Figure 2: Serial ECG tracings: A) Tracing was taken on the current presentation showing variable atrial fibro-flutter block (VR of 72), high lateral ST-segment depression (I and aVL, lime arrows), inferior pathological Q waves (III and aVF), alternative RBBB beat with type II Brugada syndrome (V1, lime arrows, blue arrows, and orange circle), and Wavy triple ECG sign or Yasser’s sign (II, V2, and V6; blue, green, and orange arrows). B) Tracing was taken within 1 min of the above ECG tracing showing variable atrial fibro-flutter block (VR of 78), ST-segment depression in aVL lead (lime arrows) with normalization of ST-segment depression in I lead (green arrows), inferior pathological Q waves (III and aVF, red arrows), alternative RBBB beat with type II Brugada syndrome (V1; lime arrows, blue arrows, and orange circles), and Wavy triple ECG sign or Yasser’s sign (II, III, V2, and V3; blue, green, and orange arrows). C) Tracing was taken within 30 days of the last 2 tracings and treatment showed controlled fixed atrial fibro-flutter block (3:1 of VR of 90; V1, pink arrows and orange circles), SISIISIII pattern (green arrows), inferior pathological Q waves (III and aVF, red arrows), and RBBB with no type II Brugada syndrome (V1, pink arrows and orange circles).