Abstract
Aim/Hypothesis: Children and adolescents with type 1 diabetes mellitus are often motivated to fast during Ramadan despite the challenges and multiple risks. This study aimed to demonstrate the impact of fasting during Ramadan on metabolic control in children and adolescents with type 1 diabetes mellitus in Tabuk city.
Methods: This prospective cross-sectional study enrolled children and adolescents aged 11–18 years with type 1 diabetes mellitus who chose to fast during Ramadan 1442/2021 (Hijri/Georgian year, 30 days). The study consisted of three stages: assessment and planning before Ramadan, daily advice and communication during Ramadan, and assessment one month after Ramadan. Details about weight, insulin dose, HbA1c, home glucose records, and type of glucose monitoring (GM) were recorded.
Results: Among 26 patients, 65% were female (35% male); 69% completed Ramadan fasting (fasting group) and 31% did not (broke-fasting group). In the fasting group, 88.9% used flash GM, whereas in the broke-fasting group, 11.1% used self-GM. The home glucose records before Iftar (sunset) were significantly different between the fasting and broke-fasting groups (p < 0.01).
Conclusion: Fasting during Ramadan in children and adolescents with type 1 diabetes mellitus is possible. Pre-Ramadan management of type 1 diabetes mellitus has a significant impact on glucose control; however, large-scale population-based studies across the country are required to further validate these results.
Keywords
adolescents, children, fasting, Ramadan, type 1 diabetes mellitus
Abbreviations
Introduction
Ramadan fasting is the fourth pillar of Islam and is obligatory for all healthy adults and adolescents. Islamic societies around the world have rituals and customs that are distinct from one another. Families and their caretakers start fasting from early dawn (Suhor) until sunset (Iftar), during which no eating or drinking is allowed. Islam has exempted several groups from fasting; however, many children and adolescents with diabetes wish to fast for the month of Ramadan, even without their physician’s permission. This attitude may be attributed to the desire to improve the feeling of self-reliance despite being having an illness and to help eliminate the sense of being physiologically different from others in the community [1].
Subsequently, pediatricians in several healthcare centers agree that adolescents may fast if they have good glycemic control, hypoglycemia symptom awareness, and frequent home glucose monitoring (GM) during the fast [2].
Children and adolescents with diabetes may be at risk of developing acute diabetes complications such as diabetic ketoacidosis and acute hypoglycemic attacks if medical advice is not followed. Therefore, it is wise to set up a protocol based on clinical and laboratory data that allow for safe and reasonable fasting during Ramadan and ensure close follow-up. Unfortunately, data in this aspect is limited, perhaps owing to the reluctance of families to allow their children to engage in such studies.
With regard to type 1 diabetes mellitus, Ramadan fasting constitutes a considerable risk for acute complications [3, 4] and is generally not advised based on studies on adults with type 1 diabetes mellitus, which categorizes them as a high-risk group for developing severe complications [5, 6].
The lack of pre-Ramadan assessment and intensive diabetes education programs are major obstacles to safe Ramadan fasting in patients with type 1 diabetes mellitus [7]. Therefore, this study aimed to demonstrate the impact of fasting during Ramadan on metabolic control in children and adolescents with type 1 diabetes mellitus in Tabuk city.
Methods
This was a prospective, cross-sectional study that enrolled children and adolescents aged 11–18 years with type 1 diabetes mellitus on multiple-dose daily insulin (basal-bolus) regimens, who choose to fast during Ramadan 1442/2021 (30 days). The exclusion criteria were diabetic ketoacidosis or episodes of hypoglycemia in the previous three months, HbA1c of more than 11, and associated autoimmune or other chronic diseases.
The first stage involved assessments and planning the fast three months before Ramadan. The patients received pre-Ramadan intensive education in the Diabetes Clinic at King Fahad Specialist Hospital in Tabuk city from a multidisciplinary team, including a pediatric endocrinologist, consultant pediatrician, diabetes educator nurse, and clinical dietitian, which included full pre-Ramadan intensive education, emphasizing how fasting affects diabetes; the insulin regimens also were identified and adjusted. Instructions on the frequency of home GM, diet, and physical exercise were also provided. Evaluation of medical history included demographic data, weight, duration of diabetes, type of home monitor, and total insulin dose per day.
The second stage of the study was during Ramadan and included daily call-free communication and follow-up advice through a social media application (Telegram), involving diet advice, insulin dose adjustment, and answering any queries via the same multidisciplinary team; pre-Iftar and pre-Suhor home GM monitoring values were obtained. In addition, patients who broke fasting were examined. The final stage assessed patients one month after Ramadan in the clinic, including weight, insulin dose, HbA1c, home GM records, and type of home GM.
Ethical approval for this study was granted by the Ethics Committee of the Ministry of Health Administration at Tabuk city. The approval included the research protocol data, collection of informed consent forms from participants, and the final report submitted at the end of the study. The reported investigations were conducted in accordance with the principles of the Declaration of Helsinki as revised in 2008. All patients or their parents/guardians provided written informed consent.
Statistical analysis
This study investigated the potential differences between the fasting and broke-fasting groups. We used non-parametric tests, such as the Wilcoxon signed-rank test for numerical variables and Fisher’s exact test for categorical variables.
The measure of the variability of the numerical variables was reported as mean ± standard deviation. Categorical variables are reported as percentages (frequencies). Statistical significance was set at p < 0.05, and R software was used for all statistical analyses (R Foundation for Statistical Computing, Vienna, Austria).
Results
In total, 26 participants were examined of which 17 were female (fasting, n = 5; broke-fasting, n = 12) and nine were male (fasting, n = 3; broke-fasting, n = 6). The mean age of participants who completed fasting was 13.25 ± 1.98 years, while that of those who broke-fasting was 13.39 ± 1.82 years. The mean history of diabetes duration was 6.500 ± 3.423 years for the fasting group and 7.444 ± 3.823 years for the broke-fasting group.
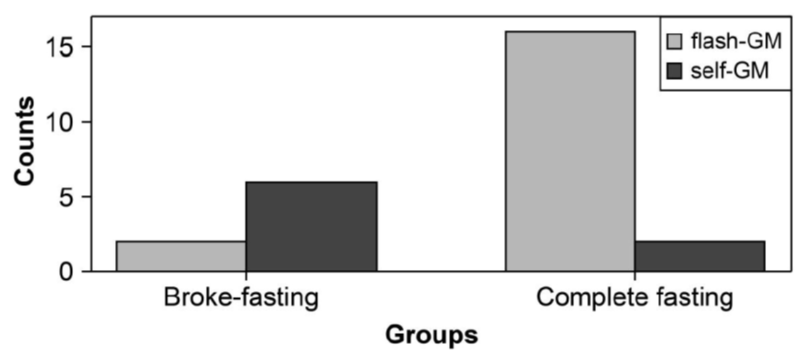
In the broke-fasting group, two participants (25.0%) used a flash-GM type of home monitor, while six participants (75.0%) used capillary fingertip pricks (self-GM). In the fasting group, 16 participants (88.9%) used a flash-GM type of home monitor, while two participants (11.1%) used self-GM. This difference in the type of home monitor used was statistically significant (p < 0.01) (Figure 1).
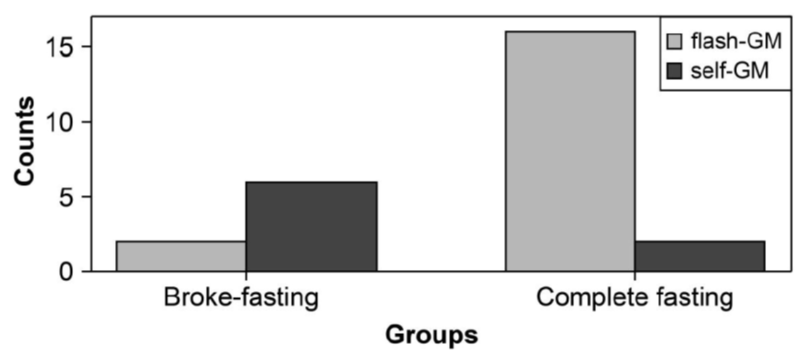
Figure 1: The difference in the type of home monitor in both groups. GM: glucose monitoring.
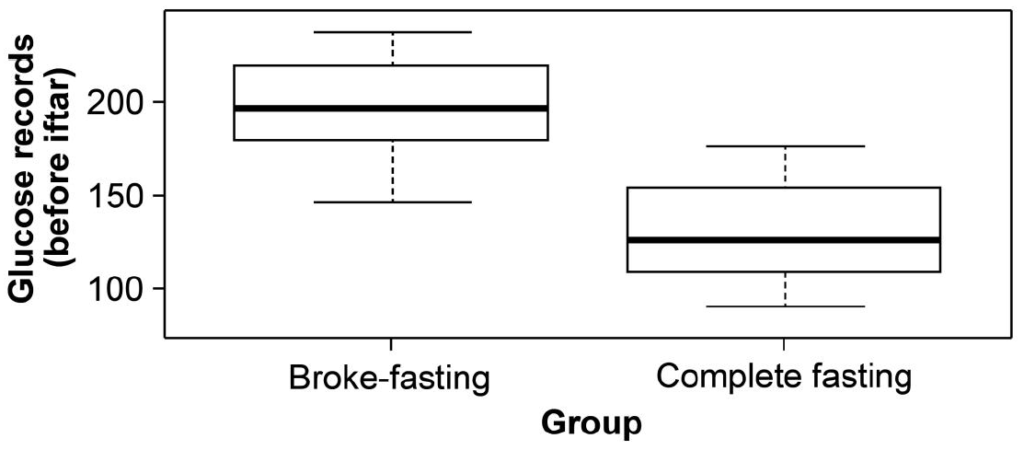
The home GM records before Iftar were significantly different (p < 0.01) between the broke-fasting and fasting groups (Table 1 and Figure 2). There were no statistically significant differences in weight, HbA1c, and total insulin use per day for the periods before and at the end of Ramadan between the two groups (Table 2 and 3).
| Variables | Broke-fasting group
(n = 8) | Fasting group
(n = 18) | P-value |
| Sex | 1.000 |
| – female | 5 (62.500%) | 12 (66.667%) | |
| – male | 3 (37.500%) | 6 (33.333%) | |
| Age | 13.250 ± 1.982 | 13.389 ± 1.819 | 0.863 |
| Duration of diabetes | 6.500 ± 3.423 | 7.444 ± 3.823 | 0.555 |
| Type of home monitor | 0.003 |
| – Flash-GM | 2 (25.000%) | 16 (88.889%) | |
| – Self-GM | 6 (75.000%) | 2 (11.111%) | |
| Gl records before Iftar* | 195.750 ± 28.308 | 127.722 ± 26.232 | 0.000 |
| Gl records before Suhor** | 161.750 ± 45.813 | 147.389 ± 28.560 | 0.337 |
Table 1: Patient characteristics stratified by group. Numerical variables are represented as mean ± standard deviation. Categorical variables are presented as n (%); statistical significance was set at p < 0.05. Gl: glucose; GM: glucose monitoring. *Iftar: sunset, **Suhor: early dawn.
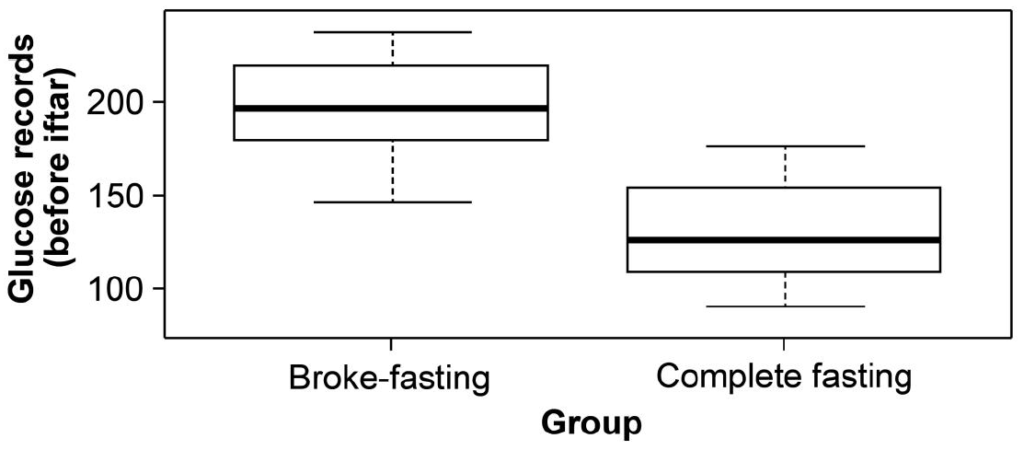
Figure 2: The glucose records before Iftar (sunset) between the broke-fasting group and fasting group.
| Variable | Period | Broke-fasting group
(n=8) | Fasting group
(n=18) | P-value |
Weight (kg) | Before Ramadan | 47.375 ± 9.694 | 43.222 ± 9.638 | 0.321 |
| End of Ramadan | 46.875 ± 9.448 | 42.944 ± 9.415 | 0.336 |
HbA1c (%) | Before Ramadan | 9.688 ± 1.223 | 9.294 ± 1.156 | 0.439 |
| End of Ramadan | 9.512 ± 1.405 | 9.222 ± 0.980 | 0.548 |
Total insulin/day
IU/day | Before Ramadan | 51.500 ± 11.006 | 48.889 ± 12.755 | 0.621 |
| End of Ramadan | 49.750 ± 14.290 | 49.667 ± 13.043 | 0.988 |
Table 2: Comparison of weight, HbA1c, and total insulin use per day before and at the end of Ramadan between groups. Numerical variables are presented as mean ± standard deviation; categorical variables are presented as n (%). Statistical significance was set at p < 0.05.
| Variable | Broke-fasting group
(n=8) | Fasting group
(n=8) | P-value |
| Weight (kg) | 0.5 ± 0.93 | 0.28 ± 0.46 | 0.457 |
| HbA1c (%) | 0.18 ± 0.36 | 0.07 ± 0.41 | 0.597 |
| Total insulin/day | 1.75 ± 7.52 | -0.78 ± 1.48 | 0.61 |
Table 3: Differences in weight, HbA1c, and total insulin use per day before and at the end of Ramadan between groups. Numerical variables are presented as mean ± standard deviation; categorical variables are presented as n (%). Statistical significance was set at p < 0.05.
Discussion
This study demonstrated that safe Ramadan fasting is possible in children and adolescents with type 1 diabetes mellitus if a comprehensive pre-Ramadan management plan—including focused education, insulin regimen adjustments, and frequent GM is ensured. Overall, 69% of the total sample population completed the fasting, which is similar to small-based population studies indicating that Ramadan fasting is a safe practice for children and adolescents with type 1 diabetes mellitus [4, 8]. Of note, there was a significant gender difference with a female predominance in the two groups however data in this aspect showed diversities and all of which were of small size sample [2, 9, 10]. Nevertheless, Ramadan fasting is still considered a risk factor for developing acute complications such as diabetic ketoacidosis and hypoglycemia, particularly in conditions of unplanned fasting [10]. The diverse observations among studies in this regard are interesting; some studies conclude that Ramadan fasting is too high a risk in patients with type 1 diabetes mellitus, advising against fasting, while others conclude that safe fasting is possible whenever pre-Ramadan management occurs [5, 6, 11].
Additionally, this study focused on the type of home GM and its effects on completing fasting during Ramadan. The main types of home GM are capillary fingertip pricks (self-GM) or self-monitoring of blood glucose, interstitial GM (flash-GM) and continuous GM (CGM). Our results demonstrated a significant difference (p < 0.003) between subjects who used flash-GM and those who used self-GM. This is the first study to examine the effect of home GM on Ramadan fasting. Interestingly, flash-GM was first evaluated as an ambulatory glucose measure during Ramadan fasting, and has been reported to provide minimally invasive yet comprehensive insight into blood glucose levels [12]. Another study reported that GM using flash-GM in children and adolescents with type 1 diabetes mellitus showed no incidence of severe hypoglycemia [13]. Furthermore, flash-GM was found to be of great value for detecting hypoglycemia in adolescents with type 1 diabetes mellitus and supported the recommendation of reducing the basal insulin dose during Ramadan to reduce the severity and duration of hypoglycemia [14]. Still, one study found that continuous GM demonstrated no difference in the mean glucose readings, or duration of hypoglycemia, hyperglycemia, and severe hyperglycemia, between the Ramadan and non-Ramadan periods; they concluded that adolescents with type 1 diabetes mellitus have varying glucose fluctuations during Ramadan [15].
Our study demonstrated significant pre-Iftar and pre-Suhor differences, between the two groups, with reference to home GM. A near optimal glucose level was observed just before ending the fast, followed by a glucose surge that lasted till dawn; this was subsequently adjusted while fasting. To the best of our knowledge, no previous studies have compared these two vital times points. A previous study evaluated the average glucose levels during the fasting vs. non-fasting periods, observing significantly lower glucose levels during the fasting period than during the non-fasting period; it was concluded that intermittent fasting could be safe for patients with type 1 diabetes [16]. In another study, theoretical evidence was found based on improvements in insulin sensitivity and a reduction in cardiovascular disease, that intermittent fasting stabilizes blood glucose levels [17].
The high pre-Suhor glucose levels reported may be due to a variety of reasons, the most noted of which, is the complexity in the pattern of carbohydrate consumption and utilization in this month. Despite no symptomatic hypo- or hyperglycemia episodes being reported among patients, blood glucose variabilities exist both at the end of and just before fasting. Another contributing factor is the change in lifestyle during Ramadan such as sleep patterns and physical activity.
No significant differences were observed regarding the HbA1c level and total insulin per day before and at the end of Ramadan between the two groups, which is consistent with similar studies [18, 19]. Moreover, the participants in both groups showed no significant difference regarding weight measurements before and at the end of Ramadan, similar to previous studies [20, 21].
Of note, as all guidelines recommended that diabetic patients should have an intensive counseling and education focusing on the need to modify medication dose and insulin timing, dietary habits, physical activity, and self-monitoring of blood sugar to reduce the risk of acute diabetic complications [22], our educational program impacted positively the success of fasting and even provide a safe broke-fasting for those who could not cope with fasting.
Although this was a prospective study, it has some limitations, mainly the small number of patients with type 1 diabetes mellitus that were included and use of data from a single center. Additionally, we focused on limited outcome measures that may be affected by other potential confounders, such as diet and physical exercise. Finally, a single measurement during the fasting month may not be enough to reflect the real impact on diabetic control, as the month of Ramadan consists of many new lifestyle experiences that require time to understand and practice.
Further, randomized clinical trials are needed to clearly define the impact of fasting on the quality of life and glycemic control. Moreover, additional research is needed with respect to fasting management plans that consider different communities and lifestyle factors during Ramadan, including dietary habits, physical activities, school demands, and the season of the year during which Ramadan falls.
Conclusion
Children and adolescents with type 1 diabetes mellitus could feasibly fast during Ramadan, provided that an intensive outpatient management program is followed. Close follow-up and frequent home monitoring are essential for successful Ramadan fasting. The type of home GM may impact fasting; however, to expand the knowledge concerning the management strategies of Ramadan fasting, larger population-based research is needed. Furthermore, high-quality studies on this subject should be given priority in Muslim‐majority countries to develop a standard of care management for children and adolescents with diabetes during the month of Ramadan.
Ethics Approval
Ethical approval for this study was granted by the Ethics Committee of the Ministry of Health Administration at Tabuk city (No.TU-077/022/117). The approval included the research protocol data, collection of informed consent forms from participants, and the final report submitted at the end of the study. The reported investigations were conducted in accordance with the principles of the Declaration of Helsinki as revised in 2008.
Patient Consent Statement
All patients or their parents/guardians provided written informed consent.
Author Contributions
La. A. Alb. formulated the study design and outlined the data for analysis, wrote the initial and final drafts of the paper, and organized the references.
- Ala. contributed to statistical analysis and results in parts and was responsible for determining the focus, type, and analysis of data, in addition to revising the manuscript, the design and presentation of the data, reviewed the contribution of the statistician, and revised the final manuscript. N. Ah. was involved in writing the main text, including the discussion; revising the contributions to the paper from other authors; reading and approving the final manuscript. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of Interest
The authors stated that they have no conflict of interest.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
References
- Jaber D, Albsoul-Younes A, Wazaify M. Physicians’ knowledge, attitude and practices regarding management of medications in Ramadan. East Mediterr Health J. 2014;20(1):56-62.
- Musleh AS, Beshyah SA, Abu Awad SM, et al. Experience with diabetic adolescents observing Ramadan fasting. Ibnosina J Med Biomed Sci. 2015;7(6):223-27.
- Salti I, Bénard E, Detournay B, et al. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27(10):2306-311.
- Al-Arouj M, Assaad-Khalil S, Buse J, et al. Recommendations for management of diabetes during Ramadan update 2010. Diabetes Care. 2010;33(8):1895-902.
- Beshyah SA. Fasting during the month of Ramadan for people with diabetes: medicine and fiqh united at last. Ibnosina J Med Biomed Sci. 2009;1(2):58-60.
- Hassanein MM. Diabetes and Ramadan: How to achieve a safer fast for Muslims with diabetes. British J Diabetes & Vascular Disease. 2010;10(5):246-50.
- Sahay R, Nagesh V. Type 1 diabetes and fasting during Ramzan. J Soc Health Diabetes. 2016;4(1):11-16.
- AlAlwan I, Al Banyan AA. Effects of Ramadan fasting on children with type 1 diabetes. Int J Diabetes Mellitus. 2010;2(2):127-29.
- Mohamed K, Al-Abdulrazzaq D, Fayed A, et al. Fasting during the holy month of Ramadan among older children and adolescents with type 1 diabetes in Kuwait. J Pediatric Endocrinol Metabol. 2019;32(8):843-49.
- Deeb A, Elbarbary N, Smart CE, et al. ISPAD Clinical Practice Consensus Guidelines: fasting during Ramadan by young people with diabetes. Pediatr Diabetes. 2020;21(1):5-17.
- Azad K, Mohsin F, Zargar AH, et al. Fasting guidelines for diabetic children and adolescents. Indian J Endocrinol Metab. 2012;16(4):516-18.
- Beshyah SA, Haddad M, Kahwatiah M. Glucose homeostasis during Ramadan fasting: first case series illustrated by flash glucose monitoring and ambulatory glucose profiling. Ibnosina J Med Biomed Sci. 2016;8(5):176-87.
- Al-Agha AE, Kafi SE, Zain Aldeen AM, et al. Flash glucose monitoring system may benefit children and adolescents with type 1 diabetes during fasting at Ramadan. Saudi Med J. 2017;38(4):366-71.
- Afandi B, Kaplan W, Majd L, et al. Rate, timing, and severity of hypoglycemia in adolescents with type 1 diabetes during Ramadan fasting: a study with Free Style Libre flash glucose monitoring system. Ibnosina J Med Biomed Sci. 2018;10(1):9-11.
- Kaplan W, Afandi B, Al Hassani N, et al. Comparison of continuous glucose monitoring in adolescents with type 1 diabetes: Ramadan versus non-Ramadan. Diabetes Res Clin Pract. 2017;134:178-82.
- Al-Ozairi E, El Samad A, Al Kandari J, et al. Intermittent fasting could be safely achieved in people with type 1 diabetes undergoing structured education and advanced glucose monitoring. Front Endocrinol. 2019;10(849):849.
- Shubrook J, Katuna J. A physician’s introduction to therapeutic fasting. Medicine Matters (Diabetes). 2019.
- Kassem HS, Zantout MS, Azar ST. Insulin therapy during Ramadan fast for Type 1 diabetes patients. J Endocrinol Invest. 2005;28(9):802-05.
- Zabeen B, Tayyeb S, Benarjee B, et al. Fasting during Ramadan in adolescents with diabetes. Indian J Endocrinol Metab. 2014;18(1):44-47.
- Karamat MA, Syed A, Hanif W. Review of diabetes management and guidelines during Ramadan. J R Soc Med. 2010;103(4):139-47.
- Bouguerra R, Jabrane J, Maâtki C, et al. La pratique du jeûne du mois de Ramadan chez le diabétique de type 2Ramadan fasting in type 2 diabetes mellitus. Ann Endocrinol (Paris). 2006;67(1):54-59.
- Suliman M, Abdu T, Elhadd T, et al. Diabetes and fasting in Ramadan: can we provide evidence-based advice to patients? Sudan Med J. 2010;46(1):4-14.