Daoud MHS 1, Elamin AEA
1, Elamin AEA *1, Ahmed A
*1, Ahmed A 2, Mohmed MHA
2, Mohmed MHA 3 and Hamid MH
3 and Hamid MH 3
3
1Department of Medicine, University of Gezira, Sudan
2Department of Physiology, Faculty of Medicine, University of Gezira, Sudan
3University of Gezira, Sudan
*Corresponding author: Abubakr Elmotesim Abdulla Elamin, Department of Medicine, University of Gezira, Sudan
Received: 18 October 2023; Accepted: 24 November 2023; Published: 01 December 2023
© 2023 The Authors. This is an open-access article and is distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Abstract
Background: This case emphasizes the atypical presentation of Ramsay Hunt syndrome (RHS), in which the rash was distributed over cervical dermatomes (C3, C4).
Case Presentation: A 55-year-old Sudanese woman presented with left-side mouth deviation and difficulty in the closure of her right eye which happened two weeks after the appearance of a vesicular rash over the right side of her head, ear, down to the right side of her neck as well as submandibular area, and improved with treatment (acyclovir and prednisolone).
Conclusion: Physicians should be aware of typical and atypical presentations of RHS to facilitate prompt diagnosis and provide appropriate management. Early intervention with antiviral and corticosteroids has been shown to significantly improve outcomes in these patients.
Keywords
Ramsay Hunt syndrome, cervical dermatomes, atypical presentation
Abbreviations
RHS: Ramsay Hunt syndrome
1. Background
Ramsay Hunt syndrome (RHS) (also called herpes zoster oticus) is a viral disease that results from the reactivation of the varicella zoster virus in the geniculate body. Typically presented with paroxysmal pain deep within the ear, LMN facial nerve palsy with vesicular rash distributed around the anterior two-thirds of the tongue, soft palate, external auditory canal, and pinna. Other cranial neuropathies might be affected and may involve cranial nerves (CNs) VIII, IX, X, V, and VI [1]. Without treatment, complete recovery occurs in about 20% of patients [2]. Combination treatment with antiviral and corticosteroids can improve outcomes in RHS if started within 72 hours [2, 3].
According to a prospective study conducted by Paul et al. [4], RHS occurs at an incidence rate of 22.4/10,000 of the population.
This case highlights the coexistence of facial palsy with cervical dermatomal involvement as an atypical presentation of RHS. The aim of this study is to inform physicians about such kind of presentation of RHS in order to facilitate prompt diagnosis and appropriate treatment.
2. Case Presentation
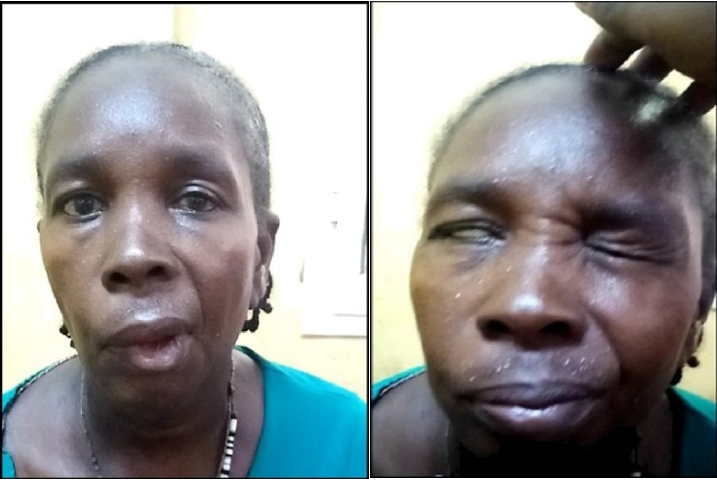
A 55-year-old Sudanese female with a clear clinical background presented to Wad Medani Teaching Hospital with left-side mouth deviation and difficulty in the closure of her right eye. Two weeks earlier, she complained of pain over the right side of her head, ear, and down to the right side of her neck, as well as the submandibular area. Then, she noticed a vesicular rash over the same area two days later. The patient sought medical advice and was diagnosed with dermatitis. Accordingly, she received topical medication and the vesicles erupted. Ten days after the rash appearance, the patient developed facial asymmetry. Clinical examination revealed hyper-pigmented skin over the right side of her neck, ear, and head (Figure 1), and also right-sided lower motor neuron (LMN) facial nerve palsy grade 5 according to the House-Brackmann facial grading system (Figure 2). Based on that, the patient was diagnosed with RHS and received acyclovir 800 mg tablets five times per day for 10 days and methylprednisolone 500 mg infusion for 5 days, followed by oral prednisolone. The patient was seen after 42 days of discharge and showed improvement with grade 3 facial palsy based on the House-Brackmann facial grading system (Figure 3) (Table 1).
 Figure 1: Hyper-pigmented skin over the right side of her neck, ear, and head.
Figure 1: Hyper-pigmented skin over the right side of her neck, ear, and head.
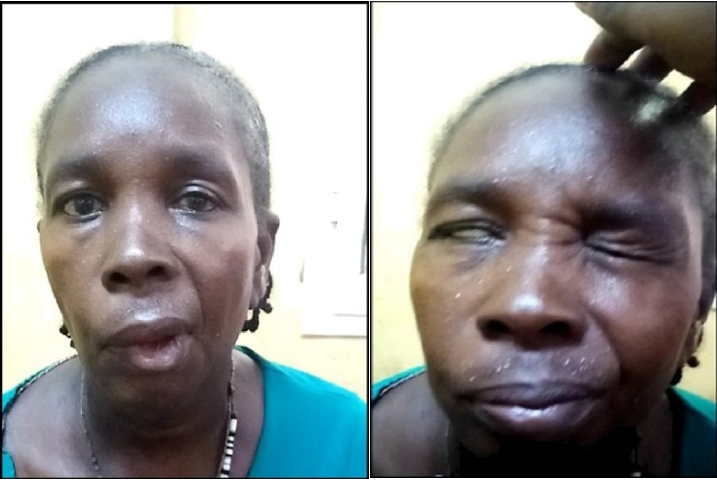 Figure 2: Right-sided facial nerve palsy grade 5 according to House-Brackmann facial grading system.
Figure 2: Right-sided facial nerve palsy grade 5 according to House-Brackmann facial grading system.
 Figure 3: Improvement with grade 3 facial palsy based on the House-Brackmann facial grading system.
Figure 3: Improvement with grade 3 facial palsy based on the House-Brackmann facial grading system.
| Time | Event |
| 2 weeks before coming to hospital | The patient complained of pain over the right side of her head, ear, and down to the right side of her neck, as well as the submandibular area. |
| 2 days later | She noticed a vesicular rash over the same area, sought medical advice, and was diagnosed with dermatitis. |
| 10 days from the rash appearance | The patient developed facial asymmetry (LMN facial palsy grade 5 according to the House-Brackmann facial grading system). |
| 10 days from the rash appearance | Diagnosis of Ramsay Hunt syndrome (RHS) is established. |
| Duration of treatment (12 days) | Received acyclovir for 10 days and methylprednisolone 500 mg infusion for 5 days followed by oral prednisolone for 7 days. |
| 42 days after treatment | Showed improvement with grade 3 facial palsy based on the House-Brackmann facial grading system. |
Table 1: Timetable for events.
3. Discussion
This case is presented with an unusual distribution of the rash, which involves cervical dermatomes (C3, C4). In comparison, Steffen et al. [5] revealed a case of RHS involving the fifth, seventh, ninth, and tenth cranial nerves, as well as the second and third cervical sensory roots or ganglia. Also, Kayayurt et al. [6] demonstrated an atypical case of RHS in a 42-year-old male with cervical nerve involvement. Another case by Worme et al. [7] revealed a case of RHS in a 54-year-old Caucasian woman with eruption of rash in the right C2-C4 dermatomes.
This atypical rash presentation may increase the risk of associated long-term nerve damage by delaying the diagnosis and consequently the management. This is exactly what happened to our case, who was initially diagnosed with dermatitis until she developed facial palsy 10 days after the appearance of the rash.
The cornerstone of managing RHS is the early empirical use of oral antiviral drugs, namely acyclovir or valacyclovir, in combination with oral steroids to improve the recovery of facial palsy [1, 8]. Acyclovir used to be the drug of choice for patients of RHS; however, new generations of antiviral medications such as valacyclovir, famciclovir, penciclovir, and brivudine are being preferred due to increasing resistance [9]. Furthermore, a high dose of intravenous methylprednisolone was found to be warranted for a successful treatment of facial nerve damage as a late treatment option [7].
We gave the patient 800 mg of oral acyclovir for 10 days and 500 mg of intravenous methylprednisolone for 5 days, followed by a short course of oral prednisolone 30 mg for an additional 7 days. Then, the patient was seen in our referral clinic 42 days post-discharge date. Her facial palsy recovered from grade 5 to grade 3 based on the House-Brackmann score. This outcome is consistent with that of the similar reported cases.
4. Conclusion
Physicians should be aware of typical and atypical presentations of RHS to facilitate prompt diagnosis and provide appropriate management. Early intervention with antivirals and corticosteroids has been shown to significantly improve outcomes in these patients.
Key Clinical Message
Vesicular rash over cervical dermatomes should be considered as atypical presentation of RHS.
Strengths
Prompt diagnosis and management of this condition led to an excellent outcome in this patient.
Limitations
Polymerase chain reaction (PCR) for varicella zoster virus (VZV) was not done because of limited resources in Sudan.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Data Availability
The data used to support the findings of this study are included within the article under references and cited throughout the body of the article with a corresponding reference in the reference list.
Funding
No funding was available.
Conflicts of Interest
The authors declare that they have no competing interests.
Author Contributions
Daoud MHS made the diagnosis of the condition. Elamin AEA assisted in writing the abstract, background, and discussion. Ahmed A assisted in writing the abstract, background, and case presentation. Hamid MH assisted in writing the case presentation. Mohmed MHA assisted in the revision of the case report and rephrasing.
Acknowledgments
Gratitude and appreciation to colleges in Wad Medani Teaching Hospital and Gezira Research Training Advocacy group for their help and support.
References
- Monsanto RD, Bittencourt AG, Bobato Neto NJ, et al. Treatment and Prognosis of Facial Palsy on Ramsay Hunt Syndrome: Results Based on a Review of the Literature. Int Arch Otorhinolaryngol. 2016;20(4):394-400.
- De Ru JA, van Benthem PP. Combination therapy is preferable for patients with Ramsay Hunt syndrome. Otol Neurotol. 2011;32(5):852-55.
- Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. 2007;44(Suppl 1):1-26.
- Paul E, Thiel T. Epidemiology of varicella zoster infection. Results of a prospective study in the Ansbach area. Hautarzt. 1996;47(8):604-09.
- Steffen R, Selby G. “Atypical” Ramsay Hunt Syndrome. Medical Journal of Australia. 1972;1(5):227-230.
- Kayayurt K, Yavasi O, Bilir O, et al. A Case of Ramsay Hunt Syndrome with Atypical Presentation. Turk J Emerg Med. 2016;14(3):142-45.
- Worme M, Chada R, Lavallee L. An unexpected case of Ramsay Hunt syndrome: case report and literature review. BMC Res Notes. 2013;6:337.
- Murakami S, Honda N, Mizobuchi M, et al. Rapid diagnosis of varicella zoster virus infection in acute facial palsy. Neurology. 1998;51(4):1202-205.
- Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. 2007;44 Suppl 1:S1-26.
![]() 1, Elamin AEA
1, Elamin AEA![]() *1, Ahmed A
*1, Ahmed A![]() 2, Mohmed MHA
2, Mohmed MHA![]() 3 and Hamid MH
3 and Hamid MH![]() 3
3